
Living with Rheumatoid Arthritis (RA) presents a multitude of challenges, and among them, foot care stands out as a critical aspect often overlooked. RA can impact the joints and tissues in your feet, leading to pain, swelling, stiffness, and mobility issues. However, with proactive care and attention, you can mitigate these effects and enhance your quality of life.
In this article, we’ll explore the journey of foot care for RA, from diagnosis to effective remedies.
Focal Points Are:
Understanding Rheumatoid Arthritis and Its Effects on the Feet:
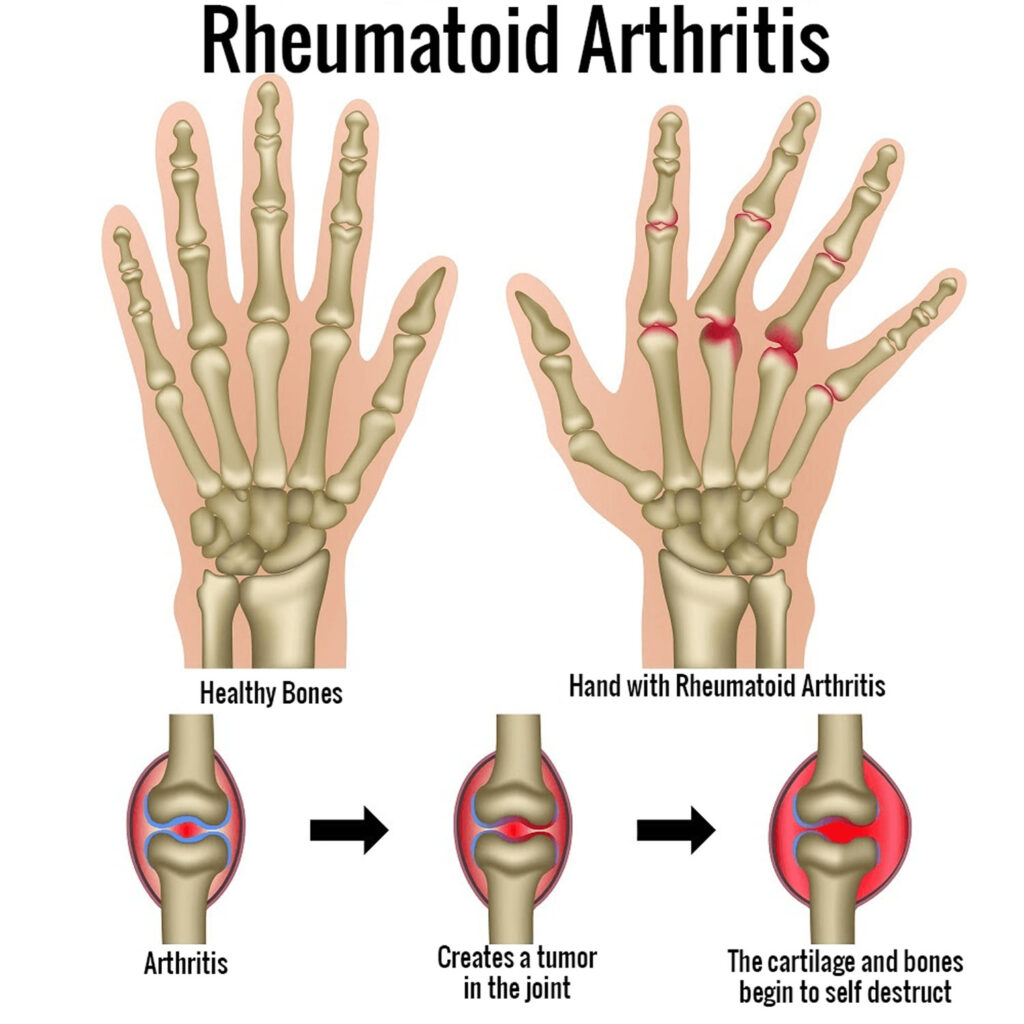
Rheumatoid Arthritis (RA) is a systemic autoimmune disease characterized by inflammation of the synovium, the lining of the joints. This chronic inflammation can lead to joint damage, deformities, and erosion of cartilage and bone over time. While RA commonly affects the hands, wrists, and knees, it can also impact the smaller joints in the feet, causing significant discomfort and impairing mobility.
The foot is a complex structure comprised of 33 joints, including the ankle, midfoot, and forefoot joints. RA can affect any of these joints, leading to a variety of symptoms and complications:
- Pain:
- Persistent pain in the affected joints is a hallmark symptom of RA.
- The pain may be dull, aching, or throbbing, and it often worsens with movement or weight-bearing activities such as walking or standing.
- Swelling:
- Inflammation associated with RA can cause swelling, also known as synovitis, in the affected joints.
- Swelling may be accompanied by warmth and redness around the joint.
- Stiffness:
- RA-related inflammation can result in stiffness, particularly in the morning or after periods of inactivity.
- Stiffness may improve with movement but can persist throughout the day, limiting flexibility and mobility.
- Limited Range of Motion:
- Joint inflammation and damage can restrict the normal range of motion, making it difficult to perform simple tasks such as bending the toes or flexing the foot.
- Reduced range of motion can further impair mobility and exacerbate functional limitations.
- Deformities:
- Over time, RA can cause structural changes in the joints, leading to deformities such as bunions, where the big toe deviates towards the other toes, or hammertoes, where the toes become bent and claw-like.
- These deformities can cause pain, difficulty wearing shoes, and alterations in gait.
- Rheumatoid Nodules:
- Some individuals with RA may develop rheumatoid nodules, which are firm lumps that form under the skin, often around pressure points or on the hands and feet.
- While usually painless, nodules can contribute to discomfort and affect the appearance of the feet.
- Secondary Conditions:
- RA-related foot problems can also predispose individuals to secondary conditions such as corns, calluses, ulcers, and infections, particularly in areas of increased pressure or friction due to deformities or altered gait patterns.
The impact of RA on the feet can significantly impair mobility, decrease quality of life, and interfere with daily activities.
Diagnosis and Assessment:
Early diagnosis is pivotal in managing Rheumatoid Arthritis (RA) effectively. If you experience persistent foot pain or notice changes in the appearance or function of your feet, seeking prompt medical attention is essential. A rheumatologist or podiatrist can conduct a comprehensive evaluation, which may include:
- Physical Examination: Your healthcare provider will perform a thorough examination of your feet, looking for signs of inflammation, deformities, or limited mobility. They may assess your gait, joint alignment, and the presence of swelling, warmth, or tenderness in specific areas. By palpating the joints and observing your range of motion, they can identify any abnormalities indicative of RA-related foot involvement.
- Imaging Tests: Various imaging modalities may be employed to visualize joint damage, erosion, or swelling in the feet:
- X-rays: X-rays can reveal changes in the bones and joints, such as joint space narrowing, erosions, or the presence of osteophytes (bone spurs). These findings can help confirm a diagnosis of RA and assess the extent of joint damage.
- Ultrasound: Ultrasound imaging can provide real-time visualization of soft tissues, including synovial inflammation, joint effusions (fluid accumulation), and tendon abnormalities. It is particularly useful for detecting early signs of RA and monitoring disease activity.
- MRI (Magnetic Resonance Imaging): MRI scans offer detailed images of soft tissues, cartilage, and bone structures in the feet. They can help identify inflammatory changes, joint damage, and complications such as tendon rupture or enthesitis (inflammation at tendon attachments).
- Blood Tests: Analysis of blood samples can aid in confirming a diagnosis of RA and assessing disease activity. Common blood tests used in the evaluation of RA include:
- Rheumatoid Factor (RF): Rheumatoid factor is an autoantibody that targets antibodies in the blood. While elevated RF levels are associated with RA, they can also be present in other autoimmune conditions and some healthy individuals.
- Anti-cyclic citrullinated peptide (anti-CCP) antibodies: Anti-CCP antibodies are more specific markers of RA and are often detected in individuals with the disease, particularly those with severe or erosive forms.
- C-reactive protein (CRP) and erythrocyte sedimentation rate (ESR): These markers of inflammation may be elevated in individuals with active RA, indicating ongoing disease activity and systemic inflammation.
By combining findings from physical examination, imaging tests, and blood work, healthcare providers can make an accurate diagnosis of RA and assess its impact on the feet. Early intervention and treatment initiation are crucial for slowing disease progression, minimizing joint damage, and improving long-term outcomes for individuals with RA.
Developing a Foot Care Plan:
Once diagnosed with Rheumatoid Arthritis (RA), collaborating with healthcare providers to develop a personalized foot care plan is essential for effectively managing the condition and maintaining foot health.

Here’s an elaboration on key components that may be included in such a plan:
- Medication Management:
- Nonsteroidal Anti-Inflammatory Drugs (NSAIDs):
- NSAIDs such as ibuprofen or naproxen may be prescribed to alleviate pain and reduce inflammation in the feet. These medications can help improve comfort and mobility, particularly during RA flare-ups.
- Disease-Modifying Antirheumatic Drugs (DMARDs):
- DMARDs, including methotrexate, hydroxychloroquine, or sulfasalazine, are often used to slow the progression of RA, reduce joint damage, and improve long-term outcomes. They work by suppressing the immune system’s abnormal response and reducing inflammation.
- Biologic Agents:
- Biologic medications, such as tumor necrosis factor (TNF) inhibitors or interleukin-6 (IL-6) inhibitors, may be prescribed for individuals with moderate to severe RA who do not respond adequately to conventional DMARDs. These drugs target specific components of the immune system involved in RA inflammation, providing targeted relief and disease control.
- Nonsteroidal Anti-Inflammatory Drugs (NSAIDs):
- Orthotics and Footwear:
- Custom orthotic inserts or supportive footwear can play a crucial role in alleviating pressure on affected joints, providing stability, and improving overall foot function.
- Orthotics are designed to distribute weight evenly, reduce stress on vulnerable areas, and correct abnormal foot mechanics associated with RA-related deformities.
- When selecting footwear, look for shoes with ample cushioning to absorb shock, wide toe boxes to accommodate deformities such as bunions or hammertoes, and good arch support to promote proper alignment and reduce strain on the feet.
- Custom orthotic inserts or supportive footwear can play a crucial role in alleviating pressure on affected joints, providing stability, and improving overall foot function.
- Physical Therapy:
- A physical therapist specializing in RA can develop a tailored exercise program to improve flexibility, strength, and balance in the feet and ankles.
- These exercises may include stretching, range-of-motion exercises, strengthening exercises, and proprioceptive training to enhance joint stability and reduce the risk of falls.
- Physical therapy sessions may also incorporate manual therapy techniques, such as joint mobilizations or soft tissue mobilizations, to alleviate pain, improve joint mobility, and enhance overall function.
- A physical therapist specializing in RA can develop a tailored exercise program to improve flexibility, strength, and balance in the feet and ankles.
- Assistive Devices:
- Assistive devices such as canes, walkers, or braces may be recommended to reduce stress on the feet and improve mobility, particularly during RA flare-ups or when experiencing severe pain.
- These devices provide additional support and stability, allowing individuals to navigate their surroundings more comfortably and safely.
- Assistive devices such as canes, walkers, or braces may be recommended to reduce stress on the feet and improve mobility, particularly during RA flare-ups or when experiencing severe pain.
- Regular Monitoring:
- Schedule regular follow-up appointments with your healthcare team, including rheumatologists, podiatrists, and physical therapists, to monitor your foot health and assess any changes or progression of symptoms.
- These appointments are essential for tracking disease activity, evaluating treatment efficacy, and making adjustments to the foot care plan as needed.
- During follow-up visits, healthcare providers may perform physical examinations, review imaging studies, and conduct blood tests to monitor disease activity and assess treatment response.
- They can also guide self-care strategies, footwear selection, and lifestyle modifications to optimize foot health and overall well-being.
- Schedule regular follow-up appointments with your healthcare team, including rheumatologists, podiatrists, and physical therapists, to monitor your foot health and assess any changes or progression of symptoms.
Regular collaboration with healthcare providers and proactive self-management are essential for achieving optimal outcomes in the management of RA-related foot complications.
Managing Flare-Ups and Pain:
Despite proactive care, Rheumatoid Arthritis (RA) flare-ups can still occur. During these times, it’s essential to prioritize self-care and manage symptoms effectively.
Here’s a detailed look at strategies to help alleviate discomfort and promote healing during RA flare-ups:
- Rest:
- Allow your feet to rest and recover during flare-ups.
- Avoid activities that exacerbate pain or inflammation, such as prolonged standing, walking long distances, or engaging in high-impact exercises.
- Opt for periods of rest and elevate your feet to reduce swelling and promote circulation.
- Consider using supportive pillows or cushions to elevate your legs while resting.
- Cold Therapy:
- Applying ice packs or cold compresses to swollen or painful joints can help reduce inflammation, numb discomfort, and provide temporary relief.
- Wrap the ice pack in a cloth or towel to protect your skin and apply it to the affected joints for 15-20 minutes at a time, several times a day, as needed.
- Be cautious not to apply ice directly to the skin for an extended period, as it can cause tissue damage or frostbite.
- Pain Management:
- Over-the-counter pain relievers such as acetaminophen (Tylenol) or nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen or naproxen sodium can help alleviate pain and discomfort during RA flare-ups.
- Follow your doctor’s recommendations for dosage and usage, and be aware of potential side effects or interactions with other medications.
- For a person with severe or persistent pain, the healthcare provider may prescribe stronger pain medications or recommend corticosteroid injections to provide targeted relief.
- Gentle Stretching:
- Perform gentle stretching exercises to improve flexibility, reduce muscle tension, and relieve stiffness in your feet and ankles.
- Focus on gentle range-of-motion exercises that target the affected joints, such as toe curls, ankle circles, or gentle foot stretches.
- Avoid overstretching or putting excessive strain on inflamed joints, and listen to your body’s signals to avoid exacerbating pain or causing further injury.
- Stress Management:
- Engage in stress-reducing activities to alleviate emotional distress, which can exacerbate pain perception and contribute to RA flare-ups.
- Practice relaxation techniques such as meditation, deep breathing exercises, guided imagery, or progressive muscle relaxation to promote calmness and reduce anxiety.
- Pursue hobbies or activities that bring joy and fulfillment, whether it’s reading, listening to music, spending time outdoors, or connecting with loved ones.

Foot care is a crucial aspect of managing Rheumatoid Arthritis effectively. By staying proactive, collaborating with healthcare professionals, and adopting healthy lifestyle habits, you can minimize the impact of RA on your feet and maintain mobility and quality of life. Remember, every step you take towards foot health is a stride towards overall well-being in your RA journey.


MOST COMMENTED
Animal-Based Proteins / Casein Protein / Dietary Protein / High-Protein Diets / Pea Protein / Plant-Based Proteins / Protein / Protein Deficiency / Protein Supplements / Proteins / Whey Protein / Whey Proteins
Is Protein Powder Safe for Teenagers and Children?
Animal-Based Proteins / Casein Protein / Dietary Protein / High-Protein Diets / Pea Protein / Plant-Based Proteins / Protein / Protein Deficiency / Protein Supplements / Proteins / Whey Protein / Whey Proteins
Unlock the Power of Proteins for Optimal Gut Health
Multivitamin
Total Health: Multivitamin for Active Lifestyles
Multivitamin
WellnessFusion: Complete Multivitamin Support
Dietary Supplement
Revitalize Your Health: The Magic of Red Yeast Rice Capsules
Foot care / Foot Health
Revitalize Your Foot Care Routine: Essential Tips for Optimal Foot Health
Foot Problem / Diabetics / Foot Health
Diabetics: Mastering Footwear Selection for Enhanced Foot Health and Ultimate Comfort
Exercises and Footwear Tips for Hammertoe Relief / Foot care / Foot Health / Foot Pain / Foot Problem / Hammertoes
Unlock Effective Exercises and Footwear Tips for Hammertoe Relief
Hammertoes / Foot Health / Foot Pain / Foot Problem
Unlock Relief: Essential Guide to Hammertoes Causes, Symptoms, and Treatments
Foot Problem / Foot Health
Revolutionize Your Recovery: Natural Remedies for Plantar Fasciitis – Fresh Home Keepers