Discover safe and effective remedies for managing constipation during pregnancy. Learn how dietary adjustments, hydration, and gentle exercise can alleviate discomfort and promote well-being for expectant mothers. Find expert tips and precautions to ensure both mother and baby’s health.
Table of Contents
Constipation and Pregnancy
Constipation is a common, albeit uncomfortable, condition that many expectant mothers face. It can cause significant discomfort and stress during what is supposed to be a joyous time. Understanding the causes, safe remedies, and when to seek medical advice are essential for managing this condition effectively.
Understanding Constipation
Causes of Constipation in Pregnancy
During pregnancy, the body undergoes significant hormonal changes that can impact the digestive system. One of the primary causes of constipation in pregnancy is the increase in the hormone progesterone. Progesterone relaxes the muscles throughout the body, including the digestive tract. This relaxation slows down digestion, allowing for increased nutrient absorption for the developing fetus but also leading to slower bowel movements and constipation.
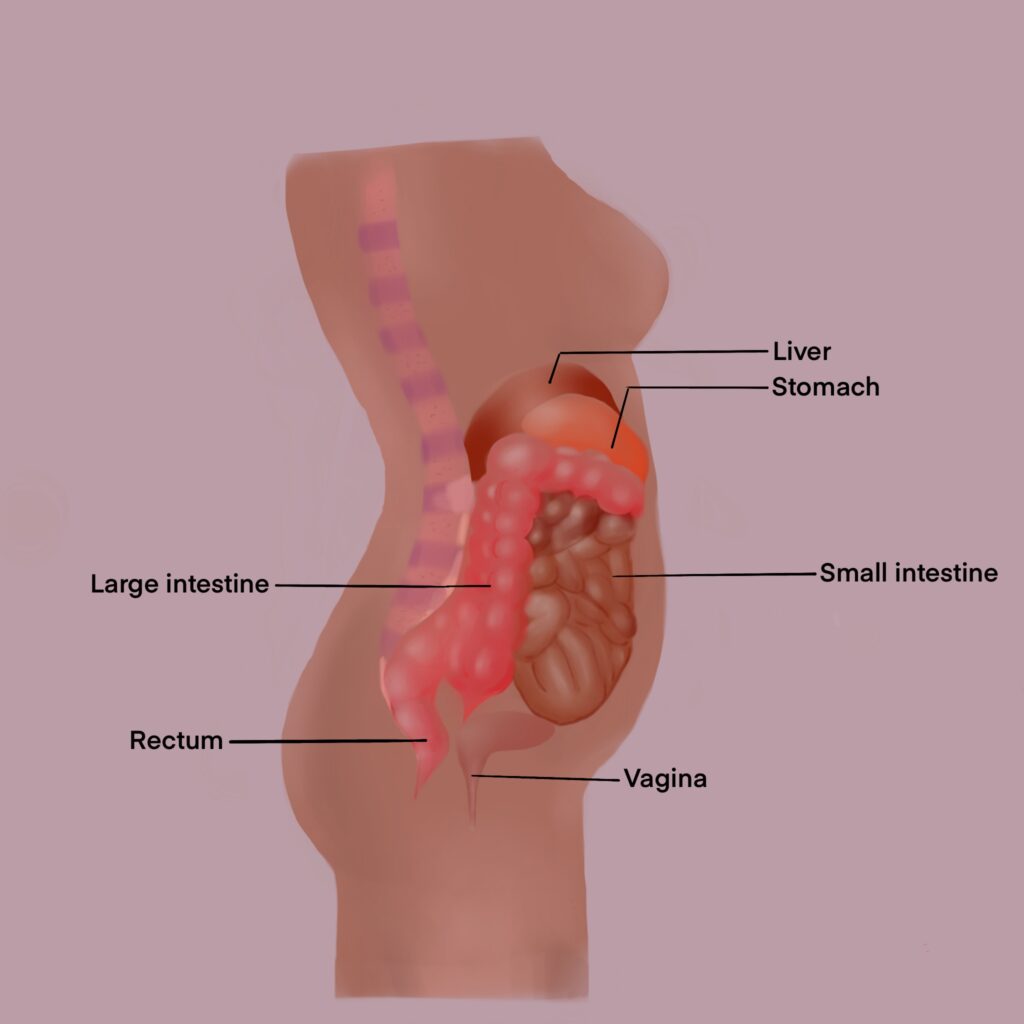
Additionally, as the pregnancy progresses, the growing uterus can exert pressure on the intestines, further impeding the normal movement of stool through the digestive tract. This physical pressure, combined with hormonal changes, contributes significantly to the occurrence of constipation during pregnancy.
Other factors that can exacerbate constipation during pregnancy include:
- Dietary Changes: Pregnant women might change their eating habits due to food aversions or cravings, which can affect digestion and bowel movements.
- Reduced Physical Activity: Many women experience fatigue during pregnancy, leading to decreased physical activity, which can slow down the digestive system further.
- Iron Supplements: Iron is crucial during pregnancy but can also cause or worsen constipation. Many prenatal vitamins contain iron, contributing to this issue.
- Dehydration: Adequate hydration is essential for softening stools and promoting bowel movements. Pregnant women may require more fluids than usual, and failure to consume enough water can lead to dehydration and constipation.
- Stress: Emotional stress can also impact gastrointestinal function, potentially leading to or worsening constipation.
How Pregnancy Affects Digestion
Hormonal Changes
One of the most profound impacts on digestion during pregnancy comes from hormonal changes, particularly the increase in progesterone levels. Progesterone, vital for maintaining the pregnancy, has a relaxing effect on the smooth muscles of the body, including those in the gastrointestinal tract. This relaxation slows down digestion, allowing for more extended nutrient absorption for the fetus but also leading to slower bowel movements and constipation.
Physical Pressure
As the uterus expands to accommodate the growing baby, it begins to exert physical pressure on surrounding organs, including the intestines and stomach. This pressure can disrupt the normal movement of food and waste through the digestive system, contributing to constipation and sometimes heartburn or indigestion. The compression of the stomach may also lead to a decrease in appetite or feelings of fullness after eating only small amounts.
Increased Blood Volume
Pregnancy significantly increases a woman’s blood volume, which can affect the digestive system. The increased blood flow to the gastrointestinal tract can alter metabolism and the way the body processes nutrients, sometimes resulting in changes to digestion and bowel habits.
Changes in Dietary and Lifestyle Habits
Pregnancy-related nausea, vomiting (especially in the first trimester), and changes in food preferences can impact dietary habits, which in turn affects digestion. Many women find themselves eating differently or struggling to maintain a balanced diet, which can exacerbate digestive issues. Additionally, fatigue and physical discomfort may lead to decreased physical activity, further slowing down the digestive system.
Increased Water Absorption
The colon absorbs more water during pregnancy, which can lead to dryer stools and, subsequently, constipation. This change is partly due to the body’s need to increase its fluid retention to support the growing fetus and amniotic fluid.
Strategies for Managing Digestive Changes
To manage these digestive changes, pregnant women are encouraged to:
- Increase fiber intake: A diet rich in fruits, vegetables, whole grains, and legumes can help improve digestion.
- Stay hydrated: Drinking plenty of water is essential for helping maintain bowel regularity.
- Exercise regularly: With a healthcare provider’s approval, regular, moderate exercise can stimulate digestion and alleviate constipation.
- Eat smaller, more frequent meals: This can help ease heartburn and indigestion.
- Limit certain foods: Reducing intake of high-fat, spicy, or highly processed foods can help reduce digestive discomfort.
Safe Remedies for Expectant Mothers
Dietary Changes
Increase Fiber Intake: Consuming a diet rich in fiber helps bulk up stool, making it easier to pass. Foods high in fiber include fruits (such as raspberries, pears, and apples with skin), vegetables (like broccoli, carrots, and Brussels sprouts), legumes (beans, lentils, chickpeas), and whole grains (oatmeal, quinoa, whole wheat bread).
Focus on Hydration: Drinking plenty of fluids, especially water, is essential to soften stools and promote regular bowel movements. Aim for at least 8-10 glasses of water a day. Incorporating water-rich fruits and vegetables can also aid hydration.
Physical Activity
Regular Exercise: Engaging in regular, moderate exercise can help stimulate digestion and alleviate constipation. Activities suitable for most pregnant women include walking, prenatal yoga, and swimming. Always consult with a healthcare provider before starting a new exercise regimen.
Over-the-Counter Solutions
Bulk-forming Agents: Supplements like psyllium may be safe for some pregnant women as they absorb water in the intestine, making bowel movements easier. However, it’s crucial to discuss with a healthcare provider before starting any over-the-counter treatments.
Stool Softeners: Products containing docusate sodium may be recommended by a healthcare provider to soften stools without stimulating contractions.
Home Remedies
Prunes and Prune Juice: Prunes are a natural laxative because they contain fiber and sorbitol, a sugar alcohol that has a laxative effect.
Warm Liquids in the Morning: Drinking warm liquids, especially on an empty stomach, can help stimulate bowel movements. A cup of warm water or herbal tea might be beneficial.
When to See a Doctor
If home remedies and lifestyle changes do not alleviate constipation, or if there are concerns about the safety of certain treatments, it’s important to consult a healthcare provider. Additionally, seek medical advice if experiencing severe discomfort, rectal bleeding, or no bowel movement for more than a week, as these could be signs of a more serious condition.
Precautions and Considerations
Avoid Certain Laxatives: Stimulant laxatives (such as senna or bisacodyl) can cause uterine contractions and should be avoided unless specifically recommended by a healthcare provider.
Mind Iron Supplements: Some iron supplements can exacerbate constipation. If constipation becomes a significant issue, discuss alternative forms of iron supplementation with a healthcare provider.
Listen to Your Body: Make changes gradually, especially when introducing new foods or exercise routines, to see how your body responds.
Home Remedies
Fiber-rich Foods
Incorporating a variety of fiber-rich foods into your diet can help soften stools and make them easier to pass. Some good sources of dietary fiber include:
- Fruits: Berries, apples (with skin), oranges, and pears.
- Vegetables: Broccoli, spinach, carrots, and Brussels sprouts.
- Legumes: Beans, lentils, chickpeas, and peas.
- Whole Grains: Oatmeal, quinoa, barley, and whole-grain breads and cereals.
Hydration
Staying well-hydrated is crucial for preventing constipation. Water helps to soften stools and supports the digestive process. Aim for at least 8-10 glasses of water a day. You can also include other fluids like:
- Herbal teas: Certain herbal teas, such as ginger or peppermint, can soothe the digestive system. However, it’s important to choose teas that are safe during pregnancy.
- Fruit and vegetable juices: Particularly prune juice, which has natural laxative properties.
Physical Activity
Moderate exercise can help stimulate the intestines and promote regular bowel movements. Safe exercises during pregnancy include:
- Walking: A daily brisk walk can be highly effective.
- Prenatal yoga: Specific poses can help stimulate the digestive tract.
- Swimming: Gentle on the body and can help relieve constipation.
Warm Liquids in the Morning
Starting your day with a warm liquid can help kickstart your digestive system. Consider:
- Warm water with lemon: This can help hydrate and stimulate digestion.
- Herbal tea: Choose a pregnancy-safe herbal tea to soothe the digestive system.
Prunes and Prune Juice
Prunes are a natural, effective remedy for constipation due to their high fiber content and the presence of sorbitol, a sugar alcohol that acts as a natural laxative.
Proper Meal Timing and Chewing
Eating smaller, more frequent meals can prevent the digestive system from becoming overloaded, and thoroughly chewing food can aid digestion and nutrient absorption.
Probiotics
Incorporating probiotic-rich foods like yogurt, kefir, and fermented foods can support gut health and promote regular bowel movements.
Mindful Relaxation Techniques
Stress can negatively impact digestion, so practices like mindfulness, meditation, or prenatal massage may help reduce stress and improve gastrointestinal function.
Adequate Sleep
Ensuring you get enough rest can help regulate the body’s natural processes, including digestion.
When to See a Doctor
Persistent Constipation
If you’ve tried home remedies, dietary changes, and increased physical activity without relief, it’s time to consult your doctor. Persistent constipation could be a sign of an underlying medical issue that needs professional evaluation.
Accompanying Symptoms
Certain symptoms accompanying constipation could indicate more serious conditions and should prompt immediate medical attention. These include:
- Severe abdominal pain: Could indicate a blockage or other serious issues.
- Blood in stool: While this can be from hemorrhoids, which are common in pregnancy, it’s essential to rule out other causes.
- Vomiting: Persistent vomiting along with constipation could indicate a gastrointestinal obstruction.
- Weight loss: Unintended weight loss during pregnancy should always be evaluated by a healthcare provider.
- Changes in bowel habits: Sudden changes, especially with pain or bleeding, need medical assessment.
No Relief from Safe Over-the-Counter Remedies
If you’ve been advised by your healthcare provider to try over-the-counter remedies and they haven’t worked, or if symptoms worsen, it’s crucial to follow up for further advice and possibly alternative treatments.
Concerns About Medication or Supplements
If you suspect that prenatal vitamins, iron supplements, or any other medications are contributing to your constipation, discuss alternatives with your healthcare provider. Never stop or change your prenatal regimen without professional guidance.
High-Risk Pregnancy
For women with high-risk pregnancies, it’s especially important to consult a doctor before trying any new remedies for constipation. What might be safe for others could pose risks depending on your specific health circumstances.
General Health and Wellness Check
Even if constipation isn’t severe, discussing it during your regular prenatal visits is a good practice. It gives your doctor a complete picture of your health during pregnancy and can help them provide the best care for you and your baby.
Guidance and Reassurance
Sometimes, just speaking with a healthcare provider can offer reassurance and personalized advice that addresses both the physical and emotional aspects of dealing with constipation during pregnancy.

Precautions and Considerations
Consult Your Healthcare Provider
Before trying any new remedy, supplement, or exercise, it’s crucial to consult with your healthcare provider. This ensures that any action taken is safe for your specific pregnancy circumstances.
Be Cautious with Over-the-Counter (OTC) Laxatives
Many OTC laxatives are not recommended during pregnancy because they can potentially stimulate uterine contractions or lead to dehydration. Always get approval from your healthcare provider before using any laxatives, including herbal or “natural” ones.
Monitor Iron Intake
Iron supplements, often prescribed during pregnancy to prevent or treat anemia, can contribute to constipation. If you suspect your iron supplement is causing constipation, discuss with your healthcare provider. They may recommend a different type of iron supplement or adjust your dosage.
Avoid Certain Foods and Medications
Some foods and medications can exacerbate constipation. Limit intake of high-fat, low-fiber foods, and be cautious with any medications or supplements not prescribed or approved by your healthcare provider.
Stay Hydrated
Dehydration can worsen constipation, so it’s important to drink plenty of fluids. While water is the best option, you can also hydrate with fruits and vegetables high in water content, as well as with soups and broths.
Gradually Increase Fiber Intake
While fiber is essential for alleviating constipation, increasing fiber intake too quickly can lead to gas, bloating, and discomfort. Gradually add fiber-rich foods to your diet and ensure you’re drinking plenty of water to help manage these side effects.
Exercise with Caution
Exercise can help manage constipation, but it’s important to choose activities that are safe during pregnancy. Consult with your healthcare provider about what exercises are appropriate for you, especially as your pregnancy progresses.
Listen to Your Body
Pay attention to how your body responds to different foods and activities. What works for one person may not work for another. If something makes you uncomfortable or worsens your symptoms, discontinue it and discuss alternatives with your healthcare provider.
Emotional Well-being
Stress and anxiety can impact digestive health, leading to or exacerbating constipation. Consider stress-reduction techniques such as prenatal yoga, meditation, or counseling to support your emotional well-being.
Conclusion
While constipation can be an uncomfortable part of pregnancy, there are many safe and effective ways to manage it. With the right approach, expectant mothers can find relief and enjoy their pregnancy journey more comfortably.
FAQs
H3: Can constipation affect pregnancy?
Constipation itself is unlikely to affect pregnancy but managing it can improve comfort and well-being.
H3: Are laxatives safe during pregnancy?
Some laxatives may be safe, but always consult with a healthcare provider before use.
H3: How often should I exercise to relieve constipation?
Moderate exercise most days of the week can help, but individual needs may vary.
H3: Can stress contribute to constipation in pregnancy?
Yes, stress can exacerbate constipation by affecting digestive processes.
H3: Are there any long-term solutions to prevent constipation during future pregnancies?
Maintaining a healthy lifestyle, including diet and exercise, can help prevent constipation in future pregnancies.


MOST COMMENTED
Animal-Based Proteins / Casein Protein / Dietary Protein / High-Protein Diets / Pea Protein / Plant-Based Proteins / Protein / Protein Deficiency / Protein Supplements / Proteins / Whey Protein / Whey Proteins
Is Protein Powder Safe for Teenagers and Children?
Animal-Based Proteins / Casein Protein / Dietary Protein / High-Protein Diets / Pea Protein / Plant-Based Proteins / Protein / Protein Deficiency / Protein Supplements / Proteins / Whey Protein / Whey Proteins
Unlock the Power of Proteins for Optimal Gut Health
Multivitamin
Total Health: Multivitamin for Active Lifestyles
Multivitamin
WellnessFusion: Complete Multivitamin Support
Dietary Supplement
Revitalize Your Health: The Magic of Red Yeast Rice Capsules
Foot care / Foot Health
Revitalize Your Foot Care Routine: Essential Tips for Optimal Foot Health
Foot Problem / Diabetics / Foot Health
Diabetics: Mastering Footwear Selection for Enhanced Foot Health and Ultimate Comfort
Exercises and Footwear Tips for Hammertoe Relief / Foot care / Foot Health / Foot Pain / Foot Problem / Hammertoes
Unlock Effective Exercises and Footwear Tips for Hammertoe Relief
Hammertoes / Foot Health / Foot Pain / Foot Problem
Unlock Relief: Essential Guide to Hammertoes Causes, Symptoms, and Treatments
Foot Problem / Foot Health
Revolutionize Your Recovery: Natural Remedies for Plantar Fasciitis – Fresh Home Keepers