Constipation is a common but uncomfortable condition affecting many pregnant women. Understanding its causes, recognizing the symptoms, and knowing how to safely relieve it are vital steps toward maintaining both maternal and fetal health during pregnancy. This article will explore the intricacies of constipation in pregnancy, offering safe and effective strategies for relief.
Table of Contents
Understanding Constipation in Pregnancy
Causes of Constipation in Pregnancy
Several factors contribute to constipation in pregnancy:
- Hormonal Changes: Increased levels of the hormone progesterone relax the muscles throughout the body, including the digestive tract. This relaxation slows down digestion, leading to constipation.
- Pressure on the Intestines: As the uterus expands to accommodate the growing fetus, it can exert pressure on the intestines, further slowing down bowel movements.
- Iron Supplements: Iron is commonly found in prenatal vitamins and is crucial for preventing anemia. However, it can also lead to constipation. Consult your healthcare provider if you believe your supplements are causing constipation; there may be alternative options.
- Diet and Hydration: Changes in diet or not drinking enough water during pregnancy can reduce the moisture content of stool, making it harder to pass.
- Reduced Physical Activity: Pregnant women might reduce their physical activity due to fatigue, discomfort, or advice to rest, which can decrease bowel motility.
Recognizing Constipation Symptoms
Symptoms of constipation include:
- Fewer than three bowel movements per week.
- Hard, dry, or lumpy stools.
- Difficulty or pain when passing stools.
- Feeling as though there’s a blockage in your intestines.
When to Seek Medical Advice
While constipation is generally not serious, it’s important to consult your healthcare provider if:
- You experience severe or persistent pain.
- There is blood in your stools.
- Constipation is accompanied by other concerning symptoms, such as vomiting or abdominal pain.
- Over-the-counter remedies and lifestyle changes do not provide relief.
Managing Constipation in Pregnancy
Managing constipation effectively involves a combination of dietary, lifestyle, and sometimes medical interventions:
- Diet: Increasing fiber intake through fruits, vegetables, whole grains, and legumes can help soften stools and promote regular bowel movements.
- Hydration: Drinking plenty of water and other fluids helps keep stools soft and easier to pass.
- Exercise: With your doctor’s approval, regular exercise like walking or prenatal yoga can stimulate digestion.
- Routine: Establishing a regular time each day for bowel movements can encourage consistency.
- Over-the-Counter Remedies: Some supplements and mild laxatives are safe during pregnancy, but always consult with your healthcare provider before starting any new medication.
Causes of Constipation in Pregnancy
Hormonal Changes
One of the primary reasons for constipation in pregnancy is the increase in the hormone progesterone. Progesterone is essential for maintaining a healthy pregnancy, but it also has the effect of relaxing muscle tissues throughout the body, including the digestive tract. This relaxation slows down the movement of food through the intestines, leading to longer digestion times and, consequently, constipation.
Physical Changes
As the pregnancy progresses, the growing uterus begins to exert pressure on the intestines and the rectum. This added pressure can restrict the normal movement of stool through the digestive tract, contributing further to constipation.
Diet and Lifestyle Factors
Diet plays a crucial role in maintaining regular bowel movements. During pregnancy, some women may consume less fiber than needed due to changes in appetite, food aversions, or nausea. A diet low in fiber can lead to harder stools that are difficult to pass.
Hydration is another critical factor. The body requires more fluids during pregnancy, and if not enough is consumed, it can result in dehydration. Dehydrated stools are harder and can exacerbate constipation.
Lifestyle changes during pregnancy, such as reduced physical activity, can also play a role. Exercise helps stimulate intestinal activity and can aid in preventing constipation, but many women might find it challenging to maintain their pre-pregnancy levels of physical activity due to fatigue, nausea, or other pregnancy-related conditions.
Iron Supplements
Many pregnant women are prescribed iron supplements to prevent anemia. While necessary, these supplements can have a side effect of causing or worsening constipation. It’s important to discuss with a healthcare provider if iron supplements seem to be the cause of constipation; there may be alternative forms or solutions to mitigate this side effect.
Symptoms and Diagnosis
Symptoms
- Fewer Bowel Movements: Experiencing fewer bowel movements than is typical for you can be an indication of constipation. While normal bowel movement frequency varies widely among individuals, going three or more days without one is generally considered constipation.
- Hard, Dry Stools: If the stool is notably hard and dry, it can indicate constipation. Such stools can be difficult to pass and may require straining.
- Straining During Bowel Movements: Needing to strain excessively to pass stool is a common symptom of constipation.
- Feeling of Incomplete Evacuation: After a bowel movement, if there’s a sensation that the bowel hasn’t been fully emptied, it might be a sign of constipation.
- Discomfort or Pain in the Abdomen: Bloating, abdominal pain, or discomfort can accompany constipation, often due to the buildup of stool or gas.
Diagnosis
Diagnosing constipation in pregnancy typically involves a combination of medical history review, physical examination, and, if necessary, additional tests. Here’s how the diagnosis may proceed:
- Medical History: A healthcare provider will ask about your symptoms, bowel movement patterns, diet, physical activity levels, and any medications or supplements you’re taking, including iron supplements, which can affect bowel movements.
- Physical Examination: A physical exam may include checking the abdomen for bloating or tenderness and a rectal exam to assess for any blockage or structural issues that might be contributing to constipation.
- Additional Tests: While not commonly required for diagnosing constipation, in some cases, further testing might be recommended to rule out other conditions. These tests could include blood tests to check for a thyroid imbalance (which can affect bowel movements) or imaging tests to look for obstructions in the colon.
Management and Relief Strategies
Upon diagnosing constipation, most treatment strategies during pregnancy focus on lifestyle and dietary modifications, such as increasing fiber intake, staying hydrated, and maintaining an appropriate level of physical activity. In some cases, over-the-counter or prescribed medications might be considered under the guidance of a healthcare provider.

Safe Relief Strategies
Dietary Adjustments
- Increase Fiber Intake: Fiber helps to bulk up and soften the stool, making it easier to pass. Include a variety of high-fiber foods in your diet, such as fruits (like berries, apples, and pears), vegetables (such as broccoli, carrots, and leafy greens), whole grains (like oatmeal, brown rice, and whole wheat bread), and legumes (beans, lentils, and chickpeas).
- Consider Fiber Supplements: If you find it challenging to get enough fiber from your diet alone, a fiber supplement may be helpful. However, it’s important to consult with your healthcare provider before starting any supplement, as they can advise the best type and dosage for your specific needs.
Stay Hydrated
- Increase Fluid Intake: Drinking plenty of fluids, especially water, can help keep the stool soft and easier to pass. Aim for at least 8-10 glasses of water a day. Other fluids like herbal teas and clear broths can also contribute to your daily fluid intake.
Exercise and Physical Activity
- Regular, Moderate Exercise: Physical activity can help stimulate intestinal activity and promote more regular bowel movements. Consider gentle exercises approved for pregnancy, such as walking, prenatal yoga, or swimming. Always check with your healthcare provider before starting or modifying your exercise routine during pregnancy.
Over-the-Counter Solutions
- Bulk-Forming Agents: These are types of fiber supplements that absorb water in the intestine to form a soft, bulky stool that’s easier to pass. Examples include psyllium and methylcellulose. They are generally considered safe during pregnancy, but you should use them under the guidance of your healthcare provider.
- Stool Softeners: Stool softeners, such as docusate sodium, can make the stool easier to pass by increasing the amount of water it absorbs. They’re usually considered safe for use during pregnancy, but it’s important to consult with your healthcare provider before taking them.
Precautions
While managing constipation, it’s crucial to avoid stimulant laxatives, which can cause contractions and are generally not recommended during pregnancy. Always discuss any medications, including over-the-counter options, with your healthcare provider to ensure they are safe for you and your baby.
When to See a Doctor
If these strategies do not relieve your constipation, or if you experience severe discomfort, it’s important to consult your healthcare provider. They can provide additional guidance, rule out other conditions, and suggest other safe treatment options.
Precautions and When to See a Doctor
Precautions
- Avoid Stimulant Laxatives: Many over-the-counter laxatives work by stimulating the intestines to contract. These can potentially lead to dehydration and imbalance in electrolytes, and in some cases, might stimulate uterine contractions. Always consult with a healthcare provider before taking any laxatives.
- Moderation with Fiber Supplements: While fiber supplements can be beneficial, it’s important to start with a low dose and gradually increase to the recommended amount to minimize gas, bloating, and cramping. Also, ensure adequate fluid intake to help the fiber work effectively.
- Be Cautious with Herbal Remedies: Some herbal teas and supplements are marketed for constipation relief. However, not all herbs are safe during pregnancy, and some could harm you or your baby. Always check with your healthcare provider before using any herbal remedies.
- Regular but Gentle Exercise: While exercise is beneficial for managing constipation, be cautious not to overdo it. Choose low-impact activities and avoid strenuous exercise unless it’s already a part of your routine and approved by your healthcare provider.
When to See a Doctor
Sometimes, despite your best efforts, constipation can become severe or could indicate an underlying condition. Here are signs that you should see a healthcare provider:
- Severe or Persistent Pain: If you experience significant abdominal pain, discomfort, or cramping that doesn’t improve with home management, it’s important to consult a doctor.
- Blood in Stool: Seeing blood in your stool or on toilet paper after wiping could indicate hemorrhoids, which are common during pregnancy but can also suggest other issues that require medical evaluation.
- No Relief from Home Remedies: If dietary and lifestyle changes do not relieve your constipation, or if you can’t have a bowel movement for more than a week, it’s time to seek professional advice.
- Nausea or Vomiting: If constipation is accompanied by nausea, vomiting, or a complete inability to keep food down, this could indicate a more serious condition and requires immediate medical attention.
- Signs of Dehydration: If you experience signs of dehydration, such as dark-colored urine, dizziness, or infrequent urination, you should consult with your healthcare provider. Proper hydration is crucial for both your health and the baby’s development.
Alternative Therapies and Their Efficacy
Acupuncture
Acupuncture involves the insertion of very thin needles into specific points on the body and is believed to balance the body’s energy. Some studies suggest that acupuncture can help alleviate constipation by promoting intestinal motility. Although research specific to pregnancy-related constipation is limited, acupuncture is generally considered safe during pregnancy when performed by a licensed practitioner. It may offer a beneficial complementary treatment for managing constipation, alongside conventional methods.
Massage Therapy
Massage therapy, particularly abdominal massage, can help stimulate the intestines and relieve constipation. Gentle massage around the abdomen can encourage bowel movement and reduce symptoms of constipation. It’s important that any massage during pregnancy is done by a professional trained in prenatal massage techniques to ensure both your safety and that of your baby.
Probiotics
Probiotics are beneficial bacteria that can improve gut health and enhance digestion. While typically not considered an “alternative therapy” in the traditional sense, probiotics can be an effective complementary approach to managing constipation. Some research indicates that certain strains of probiotics can help improve bowel movement frequency and consistency in people with constipation. Probiotic-rich foods include yogurt, kefir, and fermented foods, or they can be taken as supplements. However, it’s important to choose products that are suitable for pregnancy and to consult with your healthcare provider before starting any new supplement.
Yoga
Yoga, with its emphasis on gentle stretching and relaxation, can also be beneficial for constipation. Certain poses are designed to increase abdominal pressure and stimulate digestion, which may help alleviate constipation. Prenatal yoga classes are specifically tailored to the needs of pregnant women and can be a safe way to incorporate physical activity into your routine, aiding in constipation relief.
Herbal Remedies
While some herbal remedies are touted for their laxative properties, caution is advised during pregnancy. Herbs such as senna and cascara are stimulant laxatives and should be avoided due to potential risks during pregnancy. Other herbs, like ginger and peppermint, are generally considered safe and can aid digestion, but always consult with a healthcare provider before using any herbal remedies for constipation relief.
Efficacy and Safety
The efficacy of alternative therapies can vary widely among individuals. What works for one person might not work for another. Additionally, the safety of any therapy during pregnancy depends on individual health conditions, the stage of pregnancy, and the specific practices of the therapy. It’s crucial to have a conversation with your healthcare provider about any alternative therapies you’re considering to ensure they complement your overall pregnancy care plan safely and effectively.
Conclusion
Constipation during pregnancy is a common issue but can be managed effectively with the right strategies. By understanding its causes, recognizing symptoms, and implementing safe relief methods, pregnant women can alleviate discomfort and enjoy a healthier pregnancy.
FAQs
- Is it safe to use laxatives during pregnancy? Laxatives should be used cautiously and under the guidance of a healthcare provider, as some types may not be safe during pregnancy.
- How much fiber should I consume daily to prevent constipation during pregnancy? Pregnant women should aim for about 25 to 30 grams of fiber per day, through a combination of fruits, vegetables, whole grains, and legumes.
- Can exercise really help relieve constipation during pregnancy? Yes, regular moderate exercise can help stimulate bowel movements and relieve constipation.
- Are there any specific foods I should avoid to prevent constipation? Limiting intake of refined grains, processed foods, and high-fat foods can help prevent constipation.
- When should I be concerned about constipation during pregnancy? If you experience severe pain, no bowel movement for more than a week, or notice blood in your stools, contact your healthcare provider immediately.


MOST COMMENTED
Animal-Based Proteins / Casein Protein / Dietary Protein / High-Protein Diets / Pea Protein / Plant-Based Proteins / Protein / Protein Deficiency / Protein Supplements / Proteins / Whey Protein / Whey Proteins
Is Protein Powder Safe for Teenagers and Children?
Animal-Based Proteins / Casein Protein / Dietary Protein / High-Protein Diets / Pea Protein / Plant-Based Proteins / Protein / Protein Deficiency / Protein Supplements / Proteins / Whey Protein / Whey Proteins
Unlock the Power of Proteins for Optimal Gut Health
Multivitamin
Total Health: Multivitamin for Active Lifestyles
Multivitamin
WellnessFusion: Complete Multivitamin Support
Dietary Supplement
Revitalize Your Health: The Magic of Red Yeast Rice Capsules
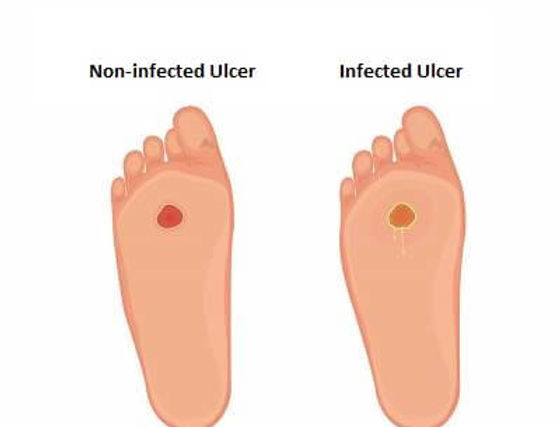
Foot care / Foot Health
Revitalize Your Foot Care Routine: Essential Tips for Optimal Foot Health
Foot Problem / Diabetics / Foot Health
Diabetics: Mastering Footwear Selection for Enhanced Foot Health and Ultimate Comfort
Exercises and Footwear Tips for Hammertoe Relief / Foot care / Foot Health / Foot Pain / Foot Problem / Hammertoes
Unlock Effective Exercises and Footwear Tips for Hammertoe Relief
Hammertoes / Foot Health / Foot Pain / Foot Problem
Unlock Relief: Essential Guide to Hammertoes Causes, Symptoms, and Treatments
Foot Problem / Foot Health
Revolutionize Your Recovery: Natural Remedies for Plantar Fasciitis – Fresh Home Keepers