Explore the comprehensive guide to Posterior Tibial Tendon Dysfunction (PTTD), from early symptoms to advanced treatment options. Learn how to manage and potentially overcome this foot condition with the latest in medical advancements and personalized care strategies.
Introduction
Posterior Tibial Tendon Dysfunction (PTTD) is a condition that can significantly impact one’s mobility and quality of life by affecting the foot’s structure and function. This guide delves into the causes, symptoms, and cutting-edge treatments for PTTD, offering hope and actionable advice for those affected. Through expert insights and personal journeys, we aim to empower individuals to navigate this condition with confidence and clarity.
Table of Contents
Overview of Posterior Tibial Tendon Dysfunction
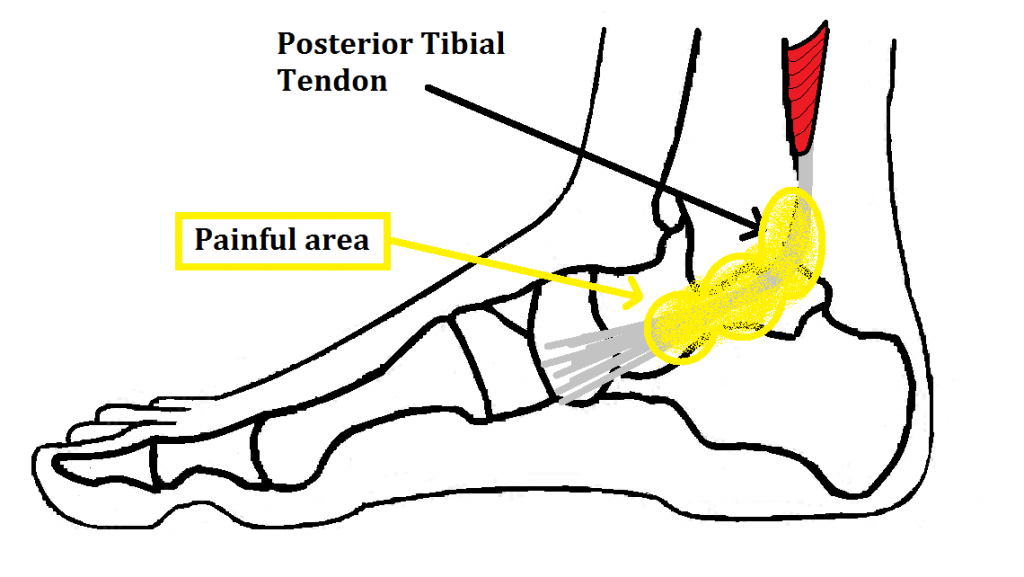
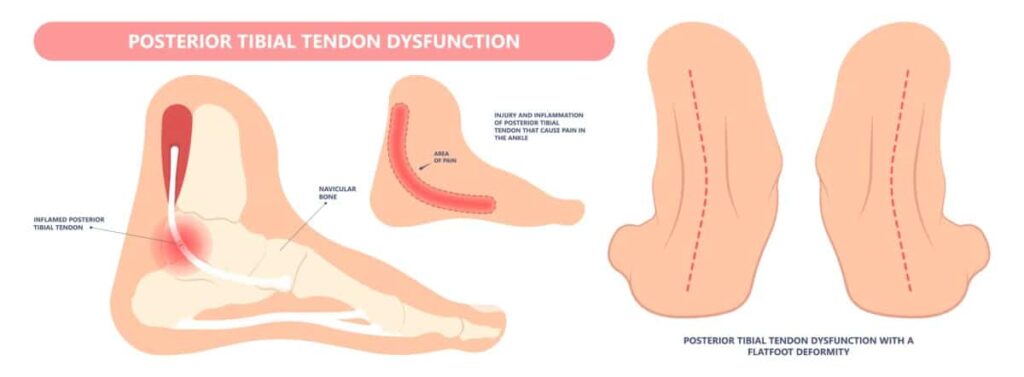
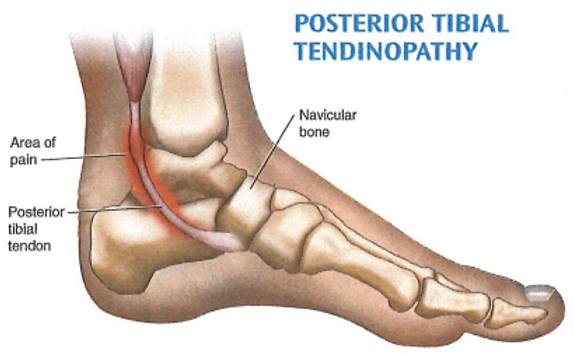
Posterior Tibial Tendon Dysfunction (PTTD) is a condition that undermines the foot’s structure and function, primarily due to the degeneration of the posterior tibial tendon. This tendon plays a pivotal role in maintaining the foot’s arch and facilitating movement. When it weakens, it leads to a progressive collapse of the foot’s arch, known as acquired adult flatfoot deformity. This condition can significantly hinder daily activities and an individual’s ability to stay active.
Causes and Risk Factors of Posterior Tibial Tendon Dysfunction
PTTD’s development is influenced by a combination of factors, highlighting the importance of awareness for prevention and timely management:
Repetitive Stress and Overuse
Athletes, dancers, and people with jobs that involve prolonged standing or walking face a higher risk due to continuous strain on the tendon.
Injury and Trauma
Direct damage to the posterior tibial tendon or ankle, including severe sprains or cumulative minor injuries, can lead to PTTD. Inadequately treated injuries are particularly problematic.
Biomechanical Issues
Those with inherent foot abnormalities, such as naturally flat feet or a pronated foot alignment, are more likely to exert extra pressure on the posterior tibial tendon, increasing the risk of dysfunction.
Systemic Health Conditions
General health issues that affect circulation and tissue integrity, like diabetes and hypertension, can weaken the tendon. Additionally, inflammatory diseases such as rheumatoid arthritis can cause inflammation and deterioration of the tendon.
Understanding these causes and risk factors is crucial for individuals at risk of PTTD, as it emphasizes the need for preventive measures and the importance of early intervention to mitigate the condition’s impact on quality of life.
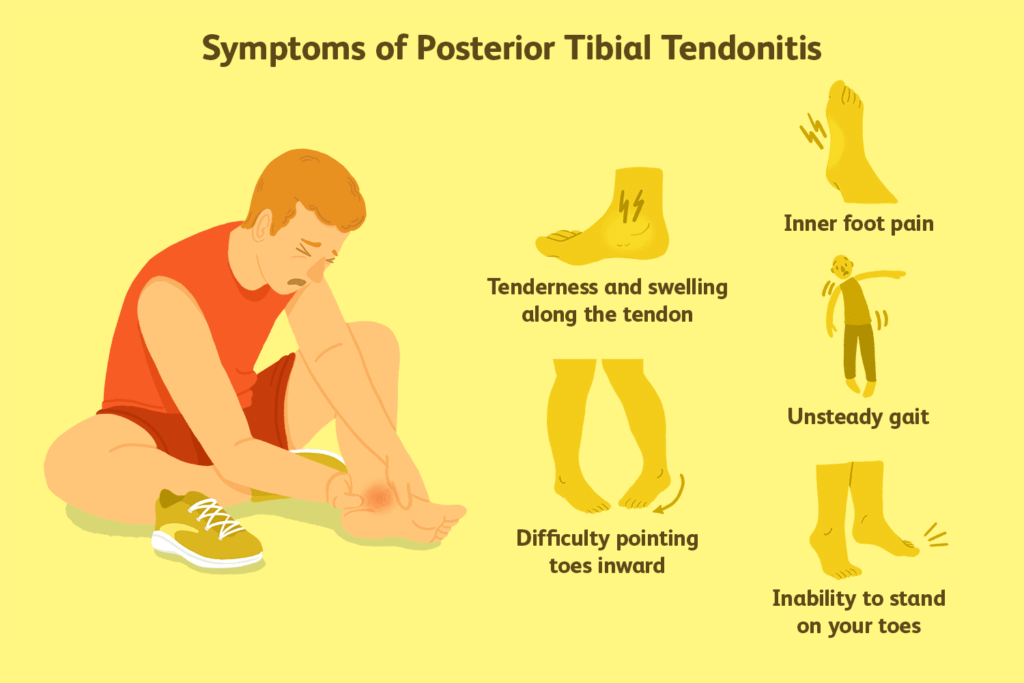
In-Depth Look at Symptoms
The progression of Posterior Tibial Tendon Dysfunction (PTTD) typically unfolds gradually, making the early detection of symptoms pivotal for effective intervention and management. Here’s a closer look at the hallmark signs and the diagnostic approach for PTTD:
Progressive Discomfort and Swelling
Pain usually starts intermittently, intensifying with physical activity and subsiding with rest. As PTTD progresses, the discomfort may become constant, significantly impacting daily functions.
Altered Foot Structure and Mobility
The slow collapse of the foot’s arch results in noticeable flattening. This structural shift can hinder the ability to stand on tiptoes and often leads to a compensatory gait to mitigate pain and instability.
Secondary Symptoms
Changes in foot architecture can trigger additional issues, including knee, hip, and lower back pain, stemming from the altered biomechanics of movement.
Diagnosis of Posterior Tibial Tendon Dysfunction
Prompt and precise diagnosis is essential to halt further tendon and structural damage. The diagnostic process generally includes:
Physical Assessment
A healthcare professional will inspect the foot for flatfoot deformity signs, swelling, and sensitivity along the posterior tibial tendon’s path. They’ll also evaluate the foot and ankle’s flexibility, strength, and alignment.
Gait Analysis
Observing how the patient walks can identify the distinctive flatfoot gait and heel tilt indicative of PTTD.
Imaging Tests
- X-rays help examine the foot’s alignment and detect structural changes associated with PTTD.
- MRI (Magnetic Resonance Imaging) offers comprehensive soft tissue images, including the posterior tibial tendon, to assess the severity of tendon damage or deterioration.
- Ultrasound might be employed to closely inspect the tendon for any signs of tears or inflammation.
Treatment Options for Posterior Tibial Tendon Dysfunction
The approach to treating Posterior Tibial Tendon Dysfunction (PTTD) is customized based on the severity and stage of the condition, focusing on alleviating discomfort, restoring functionality, and halting further progression.
Rest and Ice
Key first steps involve resting to lessen tendon strain and applying ice to reduce swelling and alleviate pain.
Orthotics
Custom orthotics play a crucial role in supporting the arch and redistributing foot pressure, which in turn, lessens the burden on the affected tendon.
Bracing
In cases of more severe tendon damage, using a brace or walking boot can provide the necessary stabilization for the foot and ankle, facilitating tendon recovery.
Physical Therapy
A specialized physical therapy regimen aims to fortify the muscles surrounding the foot and ankle, enhance mobility, and encourage tendon healing. Tailored exercises can also address and correct any abnormal walking patterns.
Medications
NSAIDs like ibuprofen or naproxen are often recommended to mitigate pain and inflammation during the condition’s acute stages.
Surgical Treatments
Should conservative measures not yield sufficient relief or if the deformity worsens, surgery might be explored. Surgical interventions can vary from tendon repair or reconstruction to procedures aimed at realigning bones (osteotomies) or fusing joints (arthrodesis) to correct the foot’s alignment and improve functionality.
Prevention Strategies for PTTD
Although complete prevention of PTTD may not always be feasible, especially for those with inherent risk factors, adopting certain strategies can lessen the risk and potentially decelerate the condition’s progression:
By understanding these treatment and prevention strategies, individuals with PTTD can take proactive steps towards managing their condition, aiming for a reduction in symptoms and an improvement in quality of life.
Weight Management
Keeping a healthy weight reduces the pressure on the posterior tibial tendon and foot structures, mitigating strain.
Choosing the Right Footwear
Opting for shoes that offer adequate arch support and cushioning can evenly distribute foot pressure, minimizing stress on the posterior tibial tendon. High heels and unsupportive shoes should be limited.
Regular Exercise
Engaging in exercises that bolster the foot and ankle’s supporting muscles and enhance flexibility can improve stability and functionality. This includes targeted exercises for the posterior tibial tendon.
Modifying Activities
Awareness of activities that excessively stress the posterior tibial tendon is crucial. Balancing high-impact activities with low-impact exercises and allowing for adequate rest can help manage tendon stress.
Frequently Asked Questions
Q: What is Posterior Tibial Tendon Dysfunction?
A: PTTD is a condition characterized by the weakening or deterioration of the posterior tibial tendon, leading to a progressive collapse of the foot’s arch, known as acquired adult flatfoot deformity.
Q: What causes PTTD?
A: Causes include repetitive stress and overuse, direct injury or trauma, biomechanical issues like flat feet, and systemic health conditions such as diabetes and rheumatoid arthritis.
Q: What are the symptoms of PTTD?
A: Symptoms typically start with intermittent pain and swelling, progressing to a noticeable flattening of the foot, difficulty standing on tiptoes, and potentially secondary symptoms like knee, hip, and back pain.
Q: How is PTTD diagnosed?
A: Diagnosis involves a physical examination, gait analysis, and imaging tests such as X-rays, MRI, or ultrasound to assess the tendon’s condition and the foot’s alignment.
Q: What treatment options are available for PTTD?
A: Treatment ranges from rest, ice, and orthotics for mild cases to physical therapy, medications, and possibly surgery for more severe cases or when conservative treatments fail to provide relief.
Conclusion
Living with Posterior Tibial Tendon Dysfunction presents its challenges, but with the right approach, it’s possible to manage the condition effectively and maintain an active lifestyle. By staying informed about the latest treatment innovations and adopting a proactive approach to foot health, individuals with PTTD can navigate their condition more successfully. This guide serves as a starting point for understanding PTTD, encouraging those affected to seek personalized care and embrace the journey toward recovery and well-being.
| Arch Support |
| Arch Supports |
| Best Arch Support Insoles |
| Best Insole for Plantar Fasciitis |
| Insole for Flat Feet |

MOST COMMENTED
Animal-Based Proteins / Casein Protein / Dietary Protein / High-Protein Diets / Pea Protein / Plant-Based Proteins / Protein / Protein Deficiency / Protein Supplements / Proteins / Whey Protein / Whey Proteins
Is Protein Powder Safe for Teenagers and Children?
Animal-Based Proteins / Casein Protein / Dietary Protein / High-Protein Diets / Pea Protein / Plant-Based Proteins / Protein / Protein Deficiency / Protein Supplements / Proteins / Whey Protein / Whey Proteins
Unlock the Power of Proteins for Optimal Gut Health
Multivitamin
Total Health: Multivitamin for Active Lifestyles
Multivitamin
WellnessFusion: Complete Multivitamin Support
Dietary Supplement
Revitalize Your Health: The Magic of Red Yeast Rice Capsules
Foot care / Foot Health
Revitalize Your Foot Care Routine: Essential Tips for Optimal Foot Health
Foot Problem / Diabetics / Foot Health
Diabetics: Mastering Footwear Selection for Enhanced Foot Health and Ultimate Comfort
Exercises and Footwear Tips for Hammertoe Relief / Foot care / Foot Health / Foot Pain / Foot Problem / Hammertoes
Unlock Effective Exercises and Footwear Tips for Hammertoe Relief
Hammertoes / Foot Health / Foot Pain / Foot Problem
Unlock Relief: Essential Guide to Hammertoes Causes, Symptoms, and Treatments
Foot Problem / Foot Health
Revolutionize Your Recovery: Natural Remedies for Plantar Fasciitis – Fresh Home Keepers