Discover the key to Constipation Relief with our comprehensive guide. Learn about effective dietary adjustments, lifestyle changes, and natural remedies designed to alleviate discomfort and improve digestive health. Unlock the secrets to a happier, healthier gut today.
Table of Contents
Introduction: Unraveling the Mysteries of Constipation
Constipation is a common ailment that affects people of all ages, yet its intricacies and solutions often remain shrouded in mystery. This guide embarks on a journey to demystify the causes of constipation and provide practical solutions. By understanding the factors that contribute to this condition, from dietary habits to lifestyle choices, we empower ourselves to make informed decisions for our health. This guide is crafted with both expertise and personal experience, aiming to be your trusted source in navigating the complexities of constipation.
Identifying the Culprits Behind Constipation
Dietary Factors: Fiber, Fluids, and Fats
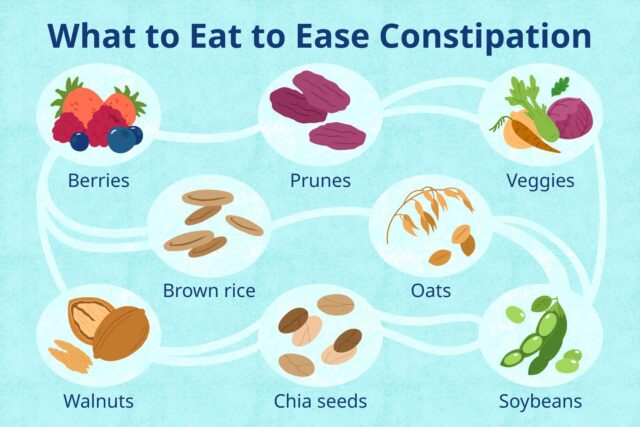
One of the primary causes of constipation is a diet low in fiber. Fiber adds bulk to the stool, making it easier to pass. Whole grains, vegetables, fruits, and legumes are rich sources of fiber that many diets lack. Inadequate fluid intake is another dietary factor. Water and other fluids help move fiber through the digestive system, facilitating smoother bowel movements. Lastly, healthy fats are essential for lubricating the intestines and promoting a healthy digestive process. Omega-3 fatty acids, found in fish, flaxseeds, and walnuts, are beneficial in this regard.
Physical Inactivity: A Silent Contributor
Lack of physical activity is another significant factor. Exercise stimulates the intestines and promotes regular bowel movements. Sedentary lifestyles, prevalent in today’s society, contribute to the slowing down of the digestive system, leading to constipation.
Medications and Supplements
Certain medications and supplements can lead to constipation as a side effect. Painkillers, antidepressants, iron supplements, and antacids containing calcium or aluminum can all reduce bowel motility. It’s essential to consult with a healthcare provider if you suspect your medication is contributing to constipation.
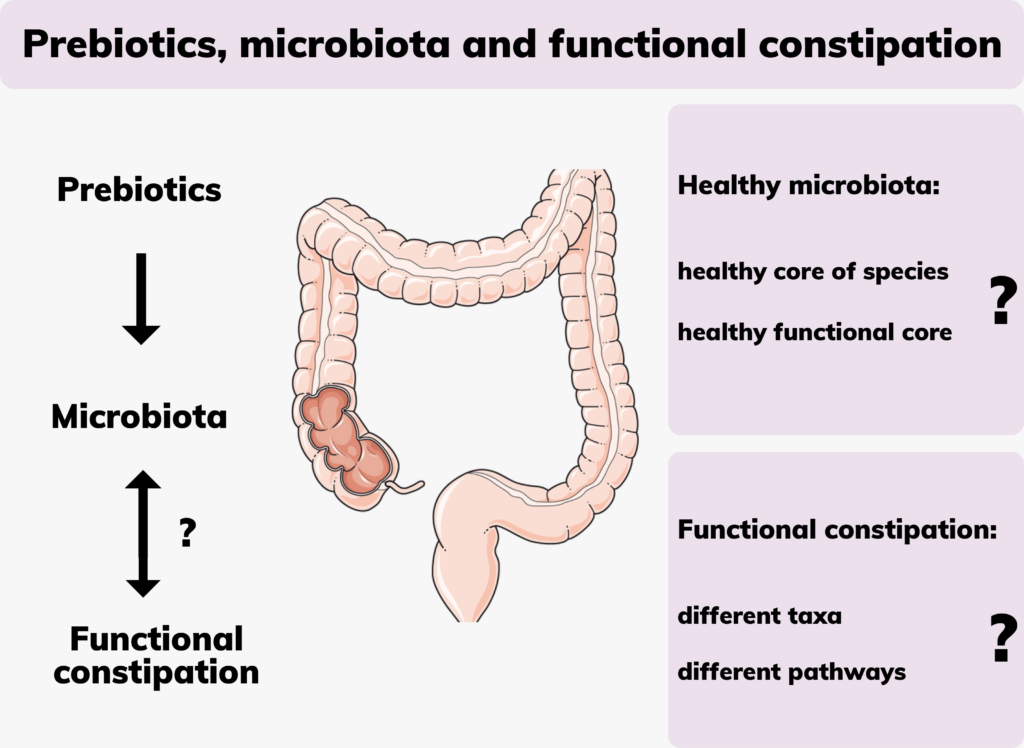
Gut Health Issues
The health of your gut plays a crucial role in preventing constipation. An imbalance in gut bacteria can lead to digestive issues, including constipation. Probiotics and a diet high in fiber can help maintain a healthy gut microbiome.
Hormonal Imbalances
Hormonal changes, such as those during pregnancy, menopause, or thyroid disorders, can affect bowel movements. These conditions can slow down the digestive system, leading to constipation.
Ignoring the Call of Nature
Frequently ignoring the urge to go to the bathroom can lead to constipation. Over time, this habit can desensitize the body’s natural signals for bowel movements, making constipation more likely.
Psychological Factors
Stress and anxiety can significantly impact digestion and lead to constipation. The body’s response to stress can slow down various bodily functions, including digestion.
Natural and Home Remedies for Relief
Hydration: One of the simplest yet most effective ways to combat constipation is to increase your water intake. Dehydration can make constipation worse. Drinking plenty of water throughout the day helps soften stool, making it easier to pass. Aim for at least 8 glasses of water daily, and consider warm liquids in the morning to stimulate bowel movements.
Dietary Fiber: Incorporating more fiber into your diet is crucial for bowel health. Fiber adds bulk to the stool and aids in its passage through the digestive system. Focus on eating plenty of fruits, vegetables, whole grains, legumes, and seeds. Foods like prunes, apples, pears, and oats are particularly beneficial for relieving constipation.
Regular Exercise: Physical activity is essential for maintaining a healthy digestive system. Exercise helps stimulate the natural contraction of intestinal muscles, facilitating the movement of stools. Even a daily 30-minute walk can make a significant difference.
Probiotics: Probiotics are beneficial bacteria that improve gut health and enhance digestion. Consuming probiotic-rich foods like yogurt, kefir, sauerkraut, and kimchi can help maintain a healthy balance of gut flora, which is vital for regular bowel movements.
Herbal Laxatives: Certain herbs have natural laxative properties that can provide short-term relief from constipation. Senna, aloe vera, and cascara are popular herbal remedies. However, they should be used with caution and not for prolonged periods, as they can lead to dependency.
Prune Juice and Dried Prunes: Prunes are well-known for their natural laxative effect, thanks to their high fiber content and the presence of sorbitol, a sugar alcohol that acts as a natural laxative. Drinking prune juice or eating dried prunes can be an effective way to relieve constipation.
Warm Lemon Water: Starting your day with a glass of warm lemon water can stimulate the digestive system and encourage bowel movements. The warmth of the water and the citrus can help hydrate and activate the bowels.
Castor Oil: This is a traditional remedy that has been used for centuries to treat constipation. It stimulates the intestines and can induce bowel movements. However, it should be used sparingly as it can cause cramping and is not suitable for everyone.
Relaxation and Stress Management: Stress can impact digestive health and contribute to constipation. Techniques such as meditation, deep breathing exercises, and yoga can help manage stress and promote relaxation, potentially easing constipation.

When to Seek Professional Help
Persistent Constipation: If you’ve tried various home remedies, dietary changes, and increased your physical activity but your constipation persists for three weeks or more, it’s time to seek medical advice. Chronic constipation could be a sign of an underlying health condition that needs to be addressed.
Blood in Stool: Noticing blood in your stool or on toilet paper after a bowel movement is a red flag. While it might be from hemorrhoids, blood in the stool can also indicate more serious conditions such as colorectal cancer or inflammatory bowel disease.
Severe Pain: If you experience significant pain during bowel movements or persistent abdominal pain, it’s essential to consult a doctor. Pain can indicate blockages, severe constipation, or other health issues that require immediate attention.
Unexplained Weight Loss: Losing weight without trying could be a symptom of a more serious underlying condition related to your digestive system. If you notice unexplained weight loss along with constipation, it’s crucial to seek professional evaluation.
Changes in Bowel Habits: Sudden changes in your bowel habits, such as alternating between constipation and diarrhea, can be a sign of a digestive disorder. If you experience significant changes that last more than a few weeks, it’s important to consult a healthcare provider.
Accompanying Symptoms: Symptoms such as unexplained nausea, vomiting, or an inability to pass gas are concerning when combined with constipation. These could indicate a bowel obstruction, which is a medical emergency.
Ineffective Over-the-Counter Medications: If you’ve tried over-the-counter laxatives or stool softeners and they haven’t provided relief, or if you find yourself increasingly reliant on them, it’s time to seek medical advice. Long-term use of some laxatives without medical supervision can lead to dependency and worsen constipation.
Family History of Colon Problems: If you have a family history of colon cancer or other gastrointestinal diseases, and you’re experiencing constipation, it’s wise to get screened. Early detection is crucial for managing these conditions.

Innovative Solutions and Therapies
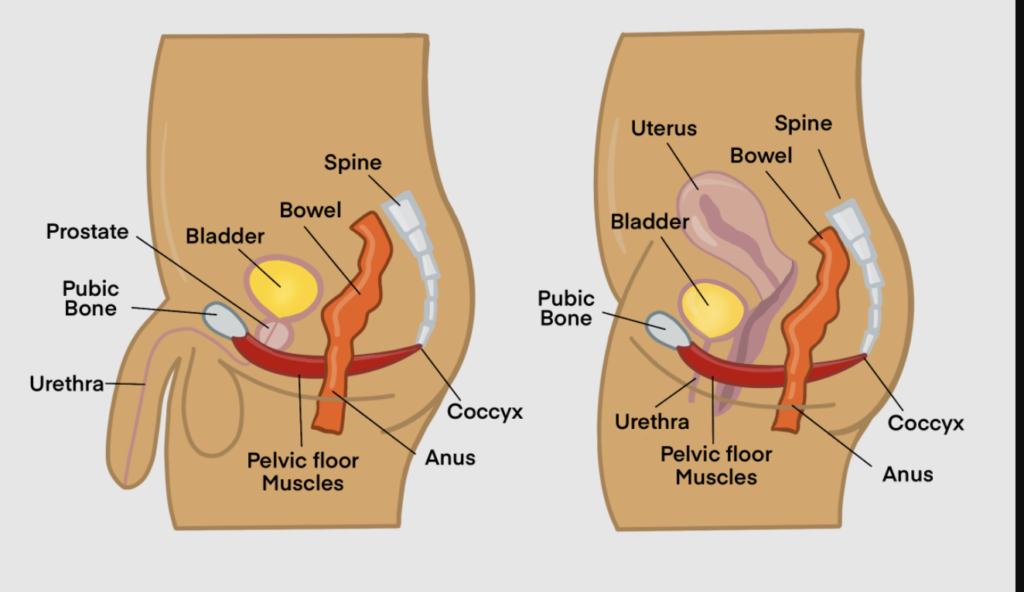
Biofeedback Therapy: Biofeedback is a non-drug treatment that teaches individuals how to control bodily functions that are normally involuntary, such as muscle contractions in the bowel. This therapy is particularly useful for individuals with chronic constipation caused by pelvic floor dysfunction. By using sensors and visual or auditory feedback, patients learn to relax and coordinate their pelvic floor muscles to improve bowel movements.
Prescription Medications: New classes of prescription medications have been developed to treat chronic idiopathic constipation (CIC) and irritable bowel syndrome with constipation (IBS-C). These include linaclotide (Linzess), lubiprostone (Amitiza), and plecanatide (Trulance), which work by increasing fluid secretion in the intestine to help speed up bowel movements. They are specifically designed for long-term use in cases where over-the-counter remedies are ineffective.
Prokinetics: Prokinetic agents are drugs that enhance gastrointestinal motility, helping to move stool through the colon more efficiently. Prucalopride is an example of a prokinetic used for the treatment of chronic constipation in individuals who do not respond to standard laxative therapies. It works by activating serotonin receptors in the gut, stimulating bowel movements.
Surgical Interventions: In rare cases, when constipation is caused by structural issues within the colon or rectum, surgery may be necessary. Procedures like subtotal colectomy (removal of part of the colon) are considered only after all other options have been exhausted and significant dysfunction or blockage is identified.
Transanal Irrigation (TAI): TAI is a therapy designed to help people with chronic constipation by introducing water into the colon via the rectum to stimulate a bowel movement. This method can be particularly beneficial for individuals with neurogenic bowel dysfunction.
InterStim Therapy: For severe cases of constipation not responding to other treatments, sacral nerve stimulation, or InterStim therapy, may be an option. This involves the surgical placement of a small device that sends electrical impulses to the sacral nerves, which are crucial for bowel control. This therapy can help improve bowel function in individuals with chronic constipation linked to nerve dysfunction.
Gut Microbiota Transplantation: Emerging research suggests that fecal microbiota transplantation (FMT) – transferring stool from a healthy donor into the gastrointestinal tract of a patient – may offer benefits for chronic gastrointestinal conditions, including chronic constipation. FMT aims to restore the balance of gut microbiota, though more research is needed to fully understand its efficacy and safety for constipation treatment.
Dietary Supplements and Functional Foods: The development of functional foods and supplements aimed at enhancing gut health is ongoing. Prebiotics and synbiotics (a combination of probiotics and prebiotics) are designed to promote the growth of beneficial gut bacteria, potentially aiding in the management of constipation.
Constipation in Special Populations
Constipation in Children
Children, particularly toddlers transitioning to solid foods or undergoing toilet training, may frequently experience constipation. This can be due to a variety of factors, including fear of using the toilet, dietary changes, and holding in stools. Treatment focuses on:
- Dietary Adjustments: Increasing the intake of fiber-rich foods and ensuring adequate hydration can help manage constipation in children.
- Behavioral Techniques: Encouraging regular toilet visits and making the bathroom a comfortable and stress-free environment can also help.
- Education: Teaching children about the importance of not ignoring the urge to use the bathroom is crucial.
Constipation During Pregnancy
Constipation is a common complaint during pregnancy, affecting up to half of all pregnant women. Hormonal changes, pressure from the growing uterus on the intestines, and the use of prenatal vitamins high in iron can all contribute to constipation. Management strategies include:
- Nutrition: Emphasizing a high-fiber diet and plenty of fluids can help alleviate symptoms.
- Exercise: Regular, moderate exercise can improve digestion and reduce the severity of constipation.
- Supplementation: With a healthcare provider’s guidance, certain supplements, such as magnesium, can be beneficial.
Constipation in the Elderly
Older adults are particularly prone to constipation due to factors like decreased physical activity, underlying medical conditions, use of medications that may cause constipation, and dietary factors. Management in the elderly requires a careful approach:
- Medication Review: Evaluating and adjusting medications that may contribute to constipation is essential.
- Diet and Hydration: Ensuring a fiber-rich diet and adequate fluid intake are foundational steps.
- Mobility: Encouraging regular physical activity, as tolerated, can help maintain regular bowel movements.
Constipation in Individuals with Neurological Conditions
People with neurological conditions such as Parkinson’s disease, multiple sclerosis, or spinal cord injuries may experience constipation due to impaired gut motility or difficulty with the physical act of defecation. Management may include:
- Specialized Care: Working with a healthcare team to address the unique challenges posed by neurological conditions.
- Adaptive Equipment: Using tools such as raised toilet seats or bidets can facilitate easier toileting.
- Tailored Medications: In some cases, medications that specifically address neurogenic bowel dysfunction may be prescribed.
Managing Constipation in Special Populations: Key Takeaways
- Individualized Approach: Tailoring constipation management to the specific needs and circumstances of each population group is crucial for effectiveness.
- Collaboration with Healthcare Providers: Close coordination with healthcare professionals can help identify the most appropriate and safe strategies for managing constipation.
- Education and Support: Providing education on dietary, lifestyle, and behavioral strategies, along with emotional and practical support, can empower individuals and caregivers to effectively manage constipation.
Preventing Constipation: Tips and Strategies
1. Increase Dietary Fiber
- What to Do: Incorporate a variety of high-fiber foods into your diet, such as fruits, vegetables, legumes, whole grains, and nuts. Aim for at least 25 to 30 grams of fiber per day.
- Why It Helps: Dietary fiber increases the bulk and softness of the stool, making it easier to pass.
2. Stay Hydrated
- What to Do: Drink plenty of fluids throughout the day. Water is best, but you can also include other beverages and hydrating foods like fruits and vegetables.
- Why It Helps: Adequate hydration helps prevent the stool from becoming hard and dry, making it easier to move through the colon.
3. Exercise Regularly
- What to Do: Engage in regular physical activity, such as walking, swimming, or cycling, for at least 30 minutes on most days of the week.
- Why It Helps: Exercise stimulates bowel movements by increasing blood flow and muscle activity in the intestines.
4. Establish a Routine
- What to Do: Try to use the bathroom at the same times each day, especially after meals, to take advantage of the natural increase in bowel activity.
- Why It Helps: Establishing a regular bowel movement routine can help train your body to have more predictable patterns.
5. Mind Your Medications
- What to Do: Review your medications with your healthcare provider to identify any that may contribute to constipation, such as opioids, antacids containing aluminum, and certain antihypertensives.
- Why It Helps: Adjusting medication use or finding alternatives can alleviate medication-induced constipation.
6. Limit Low-Fiber Foods
- What to Do: Reduce the intake of low-fiber and processed foods, such as meat, dairy, and refined grains.
- Why It Helps: These foods can contribute to constipation by slowing down bowel movements.
7. Consider Probiotics
- What to Do: Include probiotic-rich foods in your diet, like yogurt, kefir, and sauerkraut, or consider taking a probiotic supplement after consulting with a healthcare provider.
- Why It Helps: Probiotics can help balance the gut microbiome, which is essential for healthy digestion and bowel movements.
8. Manage Stress
- What to Do: Incorporate stress-reduction techniques into your routine, such as deep breathing exercises, yoga, meditation, or any activity that relaxes you.
- Why It Helps: Stress can negatively impact gut health and digestion, potentially leading to constipation.
9. Avoid Holding It In
- What to Do: Go to the bathroom when you feel the urge to have a bowel movement. Delaying can make it harder to pass stool later.
- Why It Helps: Responding promptly to your body’s signals helps maintain regular bowel movements and prevents constipation.
10. Evaluate Your Diet Supplements
- What to Do: Be cautious with iron and calcium supplements, which can contribute to constipation. Discuss with your healthcare provider if you suspect they’re causing issues.
- Why It Helps: Adjusting supplement intake or switching products may relieve constipation.
FAQ Section
- What dietary changes can help with constipation?
- How does exercise influence constipation?
- Can medication cause constipation, and what can I do about it?
- When should I seek medical help for constipation?
- Are there any new treatments for severe constipation?
- How can constipation be managed in children and the elderly?
Conclusion: Empowering Yourself to Tackle Constipation
Constipation, while common, does not have to be a constant struggle. By understanding its causes and implementing effective solutions, you can manage or even prevent this condition. Remember, your journey to overcoming constipation is a personal one, and what works for one person may not work for another. Stay informed, be proactive about your health, and don’t hesitate to seek professional help when needed. With the right approach, you can achieve relief and improve your quality of life.


MOST COMMENTED
Animal-Based Proteins / Casein Protein / Dietary Protein / High-Protein Diets / Pea Protein / Plant-Based Proteins / Protein / Protein Deficiency / Protein Supplements / Proteins / Whey Protein / Whey Proteins
Is Protein Powder Safe for Teenagers and Children?
Animal-Based Proteins / Casein Protein / Dietary Protein / High-Protein Diets / Pea Protein / Plant-Based Proteins / Protein / Protein Deficiency / Protein Supplements / Proteins / Whey Protein / Whey Proteins
Unlock the Power of Proteins for Optimal Gut Health
Multivitamin
Total Health: Multivitamin for Active Lifestyles
Multivitamin
WellnessFusion: Complete Multivitamin Support
Dietary Supplement
Revitalize Your Health: The Magic of Red Yeast Rice Capsules
Foot care / Foot Health
Revitalize Your Foot Care Routine: Essential Tips for Optimal Foot Health
Foot Problem / Diabetics / Foot Health
Diabetics: Mastering Footwear Selection for Enhanced Foot Health and Ultimate Comfort
Exercises and Footwear Tips for Hammertoe Relief / Foot care / Foot Health / Foot Pain / Foot Problem / Hammertoes
Unlock Effective Exercises and Footwear Tips for Hammertoe Relief
Hammertoes / Foot Health / Foot Pain / Foot Problem
Unlock Relief: Essential Guide to Hammertoes Causes, Symptoms, and Treatments
Foot Problem / Foot Health
Revolutionize Your Recovery: Natural Remedies for Plantar Fasciitis – Fresh Home Keepers